By Weronika Stelmach, Fourth year, Chemistry
Research suggests that psilocybin can be used as a treatment for mental illness.
Mushrooms are the umbrella shaped body of some fungi. They can be edible, as well as poisonous and sometimes psychoactive. Humans have been consuming mushrooms for all of history - including the psychedelic ones. Consuming magic mushrooms leads to perceptual change and distorted images; could this be used to treat mental illness?
In 1958, the Swiss chemist Albert Hoffman isolated psilocybin, the psychoactive compound in magic mushrooms. A new research path lit up. Studies into possible treatments for illness such as alcoholism, other addictions and schizophrenia were soon underway. During this period of research Nixon declared a war on drugs, ‘public enemy number one’. Psilocybin became a schedule 1 (class A) drug, and in 1970 all research was forced to stop.
The potentials for this drug were not forgotten, and a renaissance developed underground. Thirty years later, the first new study into psilocybin as a treatment for depression associated with terminal cancer now begins in Switzerland. This research could be more important than ever, offering the opportunity to see the full potential of what other benefits can be brought from psilocybin.
We are in a mental health epidemic. An increasing number of people suffer from mental illness, and many are not getting better. When two or more treatments fail, a patient is described as treatment resistant; often left to live with their traumas, some of which they are completely ignorant to. The mind is complicated and clever and protects you from memories which could be too painful. These memories can then creep up and affect you unexpectedly. Psilocybin treatment aims to help unlock these traumatic memories, allowing patients to process and coexist with their past.
‘More than 700,000 people die due to suicide every year.’ This statistic feels incredibly raw at Bristol University, with the many losses felt in recent years. We have seen an increased visibility and conversation about wellbeing as a result. However, personally, it feels like there’s a wall. We’re all standing behind it, looking at each other desperately. Why are we unwell? We go to the gym and eat balanced meals. We follow the advice. I want to unpick whether Psilocybin could be re-explored as a means of treating mental illness. We have got to explore new ways of treating mental illness as we are currently not making enough progress.
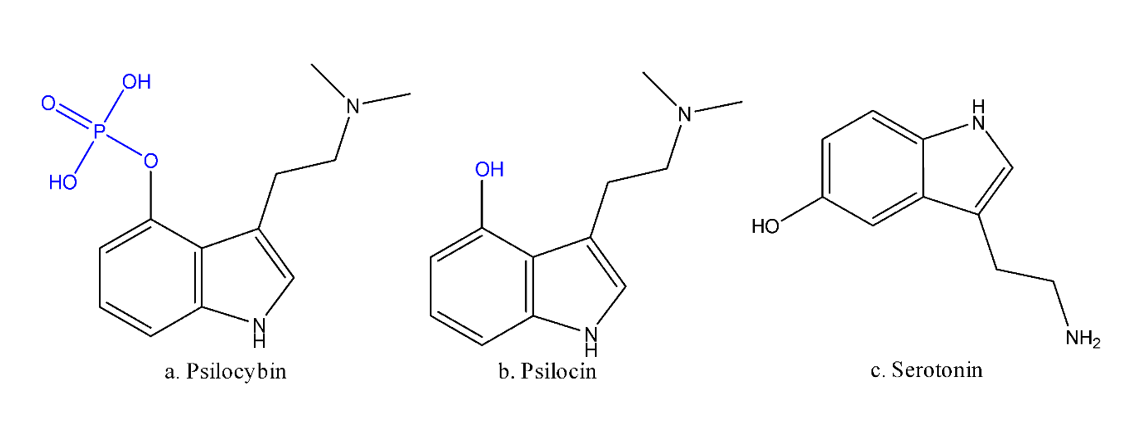
So how does it work? Psilocybin (figure 1.a) causes a change in perception, with objects taking different forms and distorted images, hallucinations. This is coupled with an increase in creativity and intensification of feeling. These changes in state may not seem like an obvious solution to mental illness, more a promotion of chaos, however these effects can be exploited. Many mental illnesses arise from a rigid and repeating cycle of brain activity. This cycle needs to be broken to get better. Psychedelics (meaning mind-manifesting in Greek) allow your neurons to have a new conversation.
When ingested, psilocybin loses its phosphorus group to become psilocin (Figure 1.b) a very structurally similar compound to serotonin (Figure 1.c), the happiness neurotransmitter.
This means that Psilocin will interact with the serotonin receptors in your brain. Most notably the 5-HT2A receptor (closely studied in psychedelic research), however several other receptors are also triggered. This allows for a loosening of neuron pathways, with new connections. This is described as a pharmacophysiological interaction, and this occurs following the effects of the drug.
The research into this has so far taken the form of a patient taking a pill of psilocybin in a controlled medical setting. The room is often decorated to be calm with music to ensure a peaceful environment. The patient is then guided through a session with a psychologist, where they can discuss and unpack the thoughts and feelings that arise.
After the initial session, measures of illness are taken at intervals directly after, and then continuously, to deduce long term effects. One of the less traditional measures is the mystical experience. The mystical experience is described as an increased feeling of dissolution of self, paired with an increased connectivity. This effect could be key to the drug's success. It provides the opportunity to step away from your problems and feel more deeply connected to your existence. One study found that 72 percent of participants had a ‘complete mystical experience’ and 67 percent stated it was one of most meaningful experiences in their lives. This could be why psilocybin has been labelled a break-through treatment by the FDA.
One of the many benefits of this treatment is the low toxicity and lack of addictiveness of psilocybin making it very safe for consumption (in a medical environment). There are always dangers with taking a substance which changes your brain functions, your experience will be deeply personal based on your past. But ultimately, this is the drugs’ biggest advantage.
The future of the field is exciting. The build-up of positive studies opens doors for more funding and loosening of restrictions. The discussion about mental health is being normalised, and with it a greater appreciation of the need for a more holistic approach into looking after our wellbeing. Could psychedelics be the sledgehammer?
Featured image: Unsplash / Mathew Schwartz