By Alejandro Ortega, Third Year, Physics and Philosophy
Bristol Medical School research examines the effect of previous interventions on HIV infections in South Africa.
The recent popular television series It’s a Sin depicts the horrific effects of the 1980s HIV/AIDS crisis on the gay community in London. Since then a lot has changed. New drugs have made it possible to live a near-normal life and new diagnoses have been steadily dropping since 2005. HIV no longer receives much attention in the UK.
However, HIV/AIDS is still highly prevalent in many countries around the world. South Africa is one of the worst affected and in 2017, nearly 25 per cent of all deaths in South Africa were attributed to AIDS. Since the virus emerged in the 1980s, South Africans have increased their use of condoms and HIV medicine.
In the past five years, the South African government has launched strategies to target HIV interventions
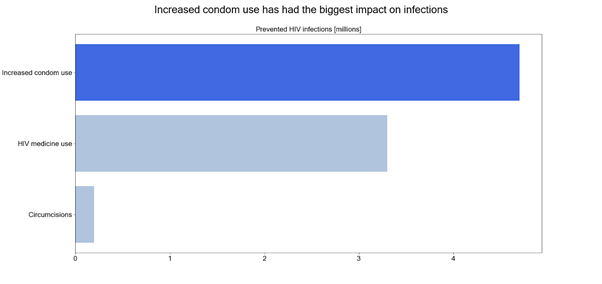
Historically, South Africa’s public health campaigns on HIV have focused on the whole population, for example on increasing general condom use. The authors of the study used a mathematical model to show that these changes have prevented millions of deaths.
Researchers additionally examined the role played by different sub-groups within the population, such as female sex workers and men who have homosexual intercourse.
The authors created the model by first obtaining relevant information about each of the sub-groups being studied. For example, they estimated the number of commercial sex clients there are in South Africa, how often on average they have sex, what proportion of the time they use condoms and what proportion of them use HIV medicine.
All of this information for each group was fed into a series of mathematical equations, which collectively modeled how HIV infections spread between all these groups. The authors then used this model to check how different interventions reduce HIV infection. For example, consider a scenario where condom use among clients increases by five per cent. By making small changes to the model, the researchers can predict if fewer people are infected with HIV.
They found that these sub-groups made disproportionate contributions to new HIV infections in the last 10 years. For example, female sex workers made up just 0.8 per cent of the population, but they contributed to 6.9 per cent of new HIV infections in the last 10 years.
‘[South Africa] may not be focusing new initiatives on those who most need them’
In the past five years, the South African government has launched strategies to target HIV interventions at female sex workers and members of the LGBT community. The study results clearly vindicate that approach.
However, researchers found that there was a particularly large contribution to HIV infections from non-commercial sex involving clients of female sex workers. That is, when men who engage with sex workers go on to have non-commercial sex with other women.
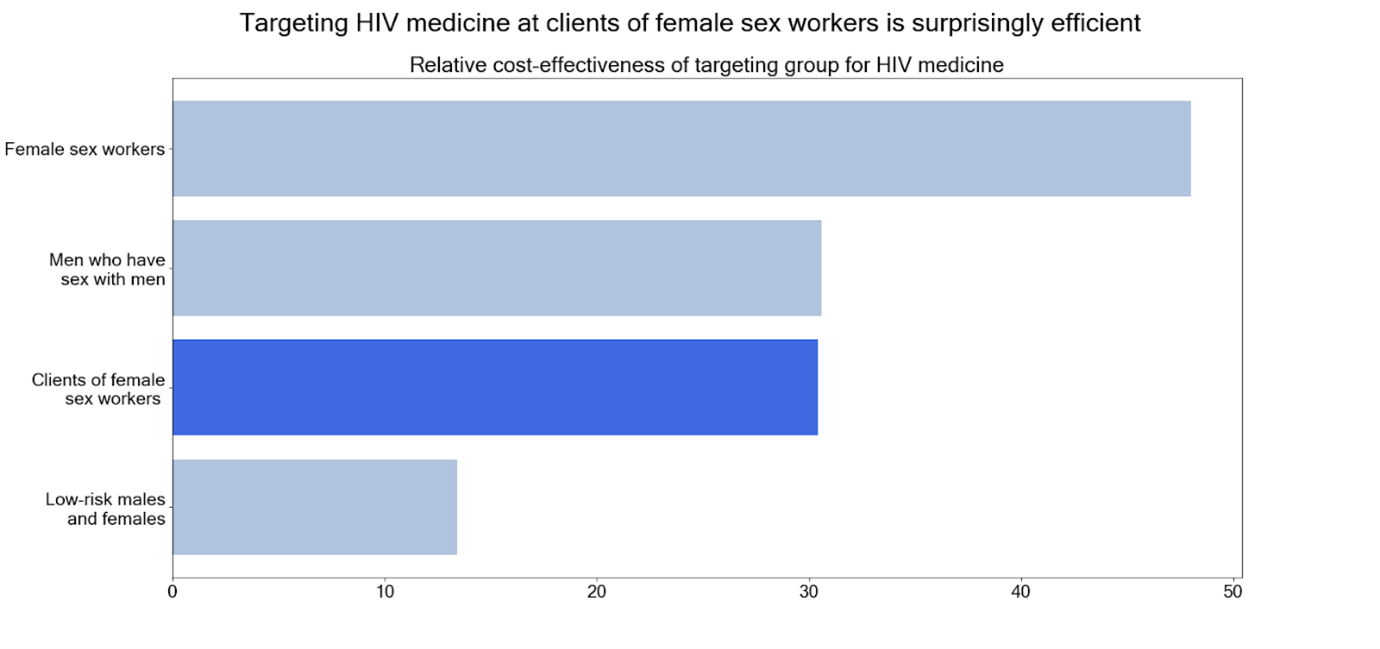
This means that to give a year’s supply of HIV medication to a client of a sex worker, would reduce new HIV infections much more than giving it to the average adult . The study suggests that clients could be targeted for HIV interventions by sex worker referral or by stationing public health officials in sex work venues.
Professor Peter Vickerman, who supervised the study, stated that: ‘South Africa, and indeed other countries, may not be focusing new initiatives on those who most need them, which, in South Africa, are the paying clients of female sex workers.’
HIV research: a 2018 update
Five films about the HIV/AIDS crisis to watch this LGBTQ+ History Month
Overall, the researchers have vindicated the strategy of targeting specific groups and make a compelling case for the future targeting of clients of sex workers. If followed through, this targeting will save many lives.
Featured Image: Pixabay / Mohamed Hassan
Has the popular television series It's a Sin changed your view on the HIV/AIDS crisis?