By Nina Bryant, Deputy News Editor
Rates of mental illness are climbing, with one in four people in the UK experiencing some kind of mental health issue. Admittedly this crisis may be greatly attributed to a lack of NHS funding, but with so many affected some clinical researchers are questioning the efficacy of conventional therapies – and investigating new leads for other treatments.
In the 50s and 60s, thousands of studies were conducted into the therapeutic use of LSD, involving over 10,000 patients. Whilst findings showed potential, research came to a halt when the recreational use of psychedelics became abundant and psychedelics became associated with hippies who broke the rules of social conformity.
Photo by Lucas Benjamin / Unsplash
As a result, psychedelic drugs such as LSD and psilocybin—the psychedelic compound in magic mushrooms—were banned in the UK in 1966. They were subsequently labelled a schedule 1 drug (i.e. a drug with no medicinal value) under the 1971 Misuse of Drugs Act. This created a huge obstacle in psychedelic research; it can take years to get a schedule 1 license and the research is more costly.
Despite this, research in this field has picked up in recent years, using drugs resembling classic psychedelics—such as synthesized psilocybin—as well as drugs with psychedelic properties such as MDMA and ketamine (a more convenient option for research given its current status as a drug with medicinal uses). Such studies have provided a lead for future research into conditions such as depression, PTSD, OCD and anxiety in terminally ill patients.
The reason psychedelics are thought to be effective in treating such conditions is that most drugs with psychedelic properties act on the same neurotransmitter as conventional antidepressants: serotonin. Drugs like MDMA mirror the psychodynamics of selective serotonin re-uptake inhibitors (SSRIs), by blocking re-uptake of serotonin, whilst drugs such as LSD and psilocybin act directly on serotonin agonists.
Professor David Nutt from Imperial College London—one of the few places conducting research into this cutting-edge field—say that scientists are still unsure why SSRIs do not produce hallucinogenic effects, given their similarities with psychedelic drugs. Professor Nutt is currently researching the use of MDMA in those with addiction to alcohol, following promising findings for the use of MDMA in the treatment of PTSD.
One of the main reasons this research is viewed as ground-breaking is the potential it offers for helping those who are ‘treatment resistant’. Both depression and PTSD are typically treated using SSRIs alongside some kind of talking therapy. However, research has indicated that both conditions may have a treatment resistance rate as high as fifty per cent.
These high rates of treatment resistance have varied explanations. For instance, for those who suffer from PTSD, reliving negative memories may trigger fear, mistrust or dissociation, thereby making therapy impossible. Interestingly, one of the ideas that propelled research in the 50s was that certain characteristics of MDMA (and indeed other psychedelic drugs) make them the ideal pharmacological treatment to facilitate psychotherapy: increased trust, decreased fear response, increasing access to repressed memories and increasing alternative ways of thinking.
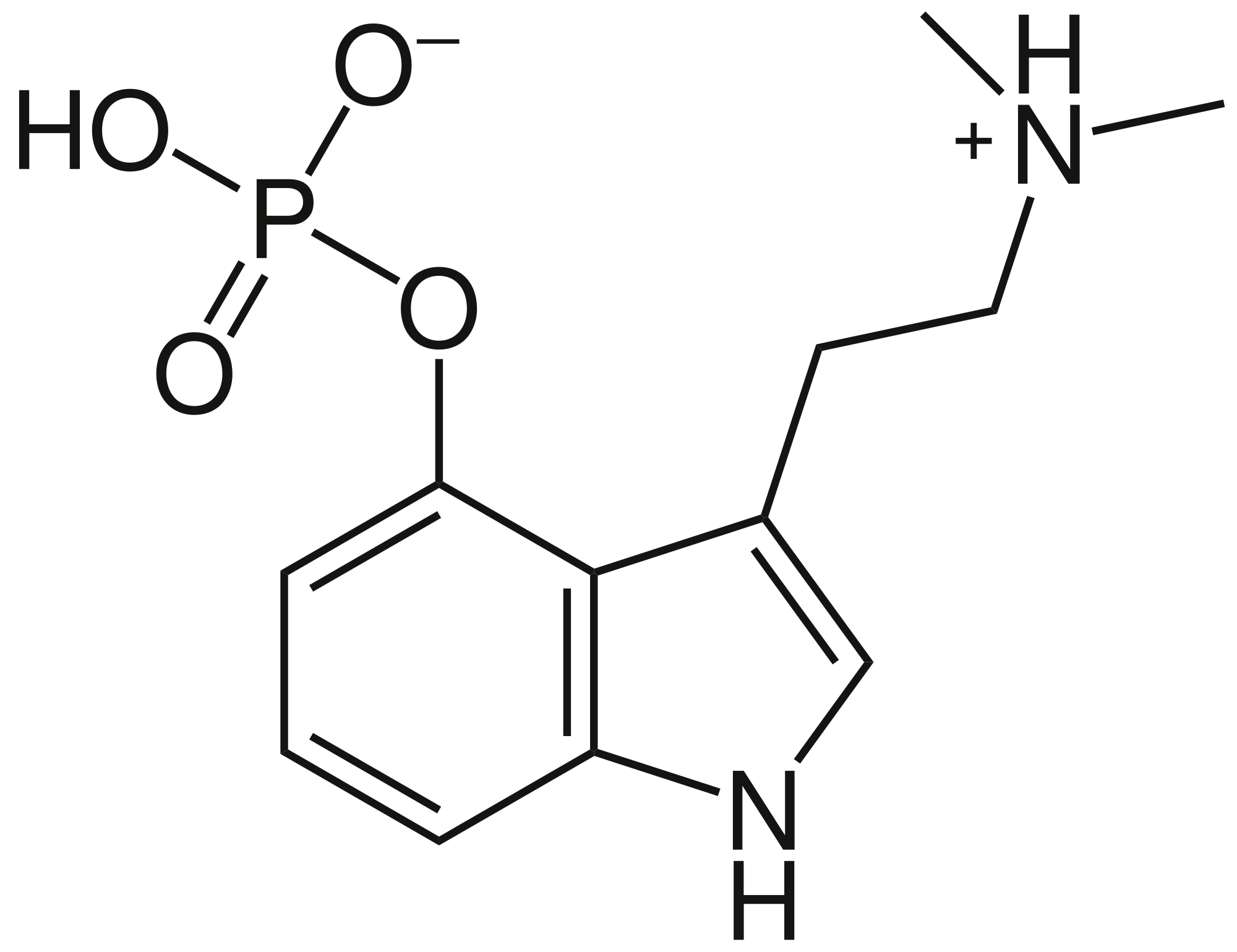
Psilocybn drug/ Wikimedia
More recently, clinical psychologist Dr Rosalind Watts from Imperial College London has advocated for the use of psilocybin as a way of addressing the root causes of problems, as opposed to SSRIs, which tend to cause emotional blunting. Whilst studies at Imperial are still in the early stages—meaning their primary aim is to test the safety of such treatments rather than the effectiveness—they have still observed greater effectiveness in those taking psilocybin than typical antidepressants, with the majority of patients maintaining a reduction in symptoms.
In terms of cost-effectiveness, it remains unclear whether the use of psychedelics would save money in terms of mental health treatment. Whilst there is a possibility that such treatment could have curative rather than alleviatory effects—meaning treatment required may be short-term—most researchers say that such treatment would have to be used alongside the supervision of a clinical psychologist in order to be effective.
Regardless of the cost-related specifics, the results of recent drug trials are of great interest to clinical researchers and psychedelic treatment campaigners. Campaigns such as ‘Psychedelics for Mental Health’ hope to see rescheduling of drugs such as LSD, psilocybin and MDMA to schedule 2 drugs in order to improve efficiency of research in this field.
Featured Image: Lucas Benjamin/ Unsplash
Should more research be carried out into psychedelics? Let us know your thoughts!