By Will Smears, Third year, Biochemistry
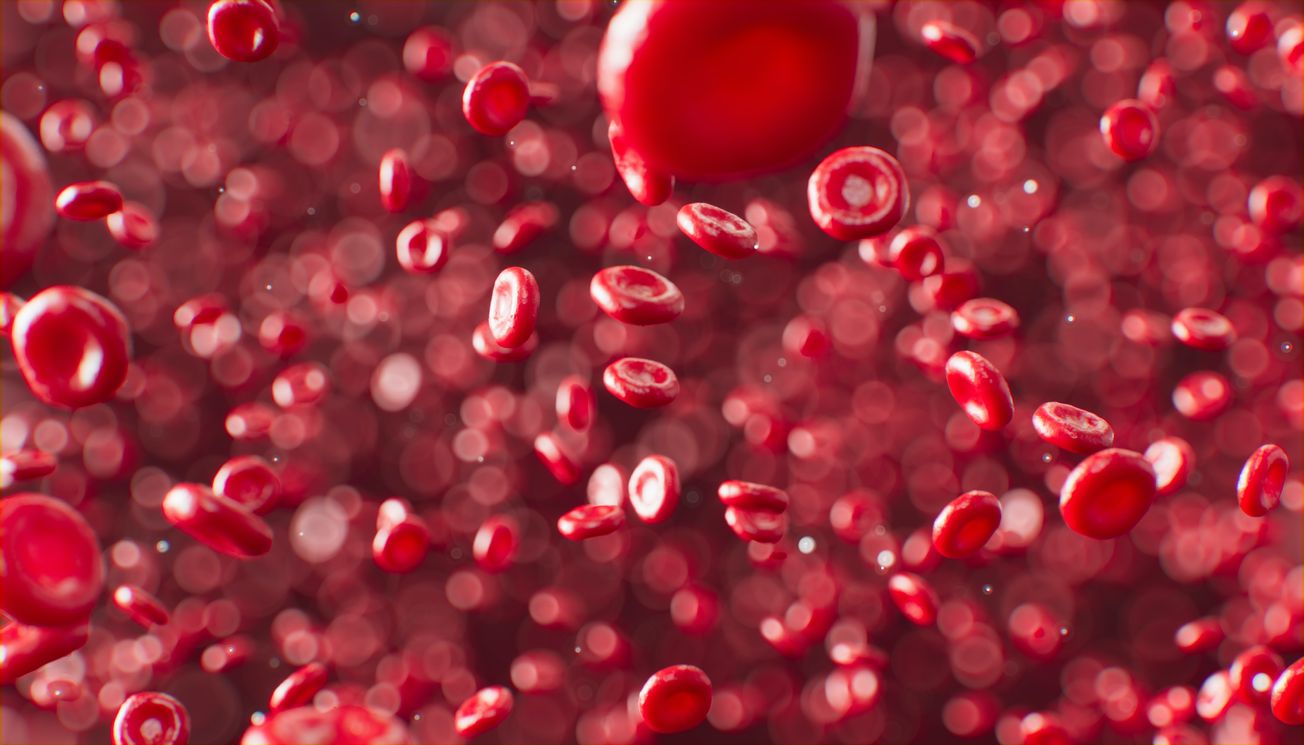
There is high demand for new blood transfusion technology, to cater to patients with rare blood types that don’t respond well to usual treatments. Researchers at the University of Bristol have created an exciting new therapy in which red blood cells are grown in the lab, which is currently under clinical trial.
Blood disorders such as Sickle Cell Disease and Thalassemia are among the most prevalent and life-threatening diseases, notably in the global south. Patients require regular transfusions from multiple donors which is highly problematic. It enables the immune system to create defensive mechanisms against a variety of blood types, triggered by the sugars and proteins coating the surface of the red blood cells.
Each of us has a unique composition of these molecules (blood type) which presents a challenge in the progression of this technology. Variety in blood groups is owed to evolution, which has encouraged changes in cell surface molecules to protect from invasive parasites, like Malaria.
Ashley Toye, Professor of Cell Biology at the School of Biochemistry is part of ongoing clinical trials which are combating this problem head-on. He is working on growing immortalised red blood cells in the laboratory which evade triggering the immune response. Immortalisation allows cells to continually divide in the body. His lab uses innovative techniques involving targeting the cells with a virus containing part of a cancer-causing gene for immortalisation.
Red blood cells grown in a lab have been transfused into another person in a world first #RESTORE trial by @NHSBT Cédric Ghevaert & @AshToye_Bristol which could revolutionise treatments for blood disorders such as #sickle cell & rare blood types.
— University of Bristol (@BristolUni) November 7, 2022
👉🏽 https://t.co/thAw63aZr1 pic.twitter.com/bV4W9s5f0j
The trials aim to study the lifespan of these red blood cells compared to normal red blood cells. It’s hoped that the lab-grown blood cells last significantly longer, thus providing therapeutic effects while omitting the requirement for regular transfusions.
The RESTORE trials are being performed in conjunction with the NHS Blood and Transplant (NHSBT), University of Cambridge, Guy’s and St Thomas’ NHS Foundation Trust, NIHR Cambridge Clinical Research Facility, and Cambridge University Hospitals NHS Foundation Trust. A grant was also provided by the National Institute for Health and Care Research. The trial is currently recruiting participants.
Yvonne Smith, a Suffolk resident, is one of the first ever people to receive lab-grown red blood cells through this trial. Her and other participants are initially transfused with either normal red blood cells or the lab-grown variety. The catch is, they don’t know which. Participants are then transfused with the alternative to determine which lasts longer.
Yvonne says the clinicians explained that ‘They wouldn’t be doing it if there was a good chance something would go awry’ and encourages ‘anybody to do it’. She explained her willingness to participate as ‘the research could help people with sickle cell and other diseases where it’s difficult to find matching blood. Otherwise, those people have a raw deal.’ So far, participants in the trial haven’t experienced any side effects.
Professor Toye and the other clinicians hope that in the future, these lab-grown cells will provide a more dependable assistance to those who struggle with blood disorders. It also shows promise in research into how parasites invade normal red blood cells. Lab-grown cells are amenable to genetic manipulation, to provide personalised blood-typed transfusions to those with rarer blood types. This may transform the lifestyle of Sickle-Cell and Thalassemia patients.
Featured image: Unsplash/Anirudh