By Katie Fulford, Second Year, Medicine
Following Epigram's investigation into hidden disabilities in the student community, Katie interviews one medical student fundraising for a chance for change
There are many different feelings and sensations that we experience as pain every day: pinching, crushing, stomach in knots, pricking. We have turned to a myriad of metaphorical terms to try and convey not only the severity or sensations of pain but also encompass the emotional consequences. But what is pain biologically?
Pain is a synaptic response of electrical signals sent to alert the brain when there is damage to the body. Typically, that pain is described as acute, and serves a biological function; warning the body of potentially harmful stimuli or injury. Pain indicates us to let our leg rest after a sprain or to let go of the hot tray when we forget to use oven gloves. However, in certain circumstances, pain can persist beyond the normal time of healing, clinically defined as more than 3 months.
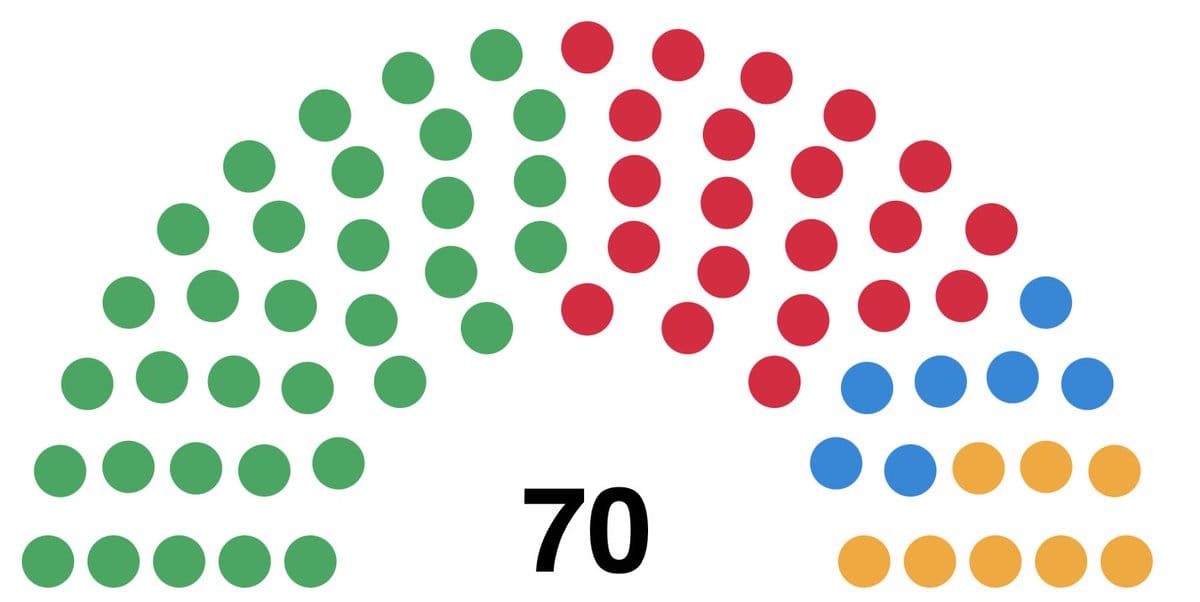
12 per cent of the UK suffer high-impact chronic pain, which means their ability to take part in daily activities is limited
Unfortunately, chronic pain is not uncommon; 35-51 per cent of the UK live with chronic pain. 12 per cent suffer high-impact chronic pain, which means their ability to take part in daily activities is limited.
Chronic pain is often resistant to treatments and instead approaches focus on resilience, emotional support systems and rehabilitation to help a patient manage the pain rather than eliminate the root of the pain itself.
The limitations chronic pain can impose can have serious psychological impacts for a person, and clinical studies have revealed that up to 85 per cent of patients with chronic pain are affected by severe depression.
University of Bristol’s Senior Research Associate, Dr Robert Drake, has recently been awarded around £300,000 in fellowship funding for his research focussing on how injury can affect brain function causing chronic pain. By looking into the wider brain network that supports emotional reactivity, coping behaviour and sensory hypersensitivity, Dr Drake hopes to shed light on how wider psychosocial factors impact how we experience pain.
George’s Story

George, a second year medical student in Bristol, has been suffering with a chronic pain condition, known as Occipital Neuralgia, ever since a rugby injury five years ago. The condition, which leaves George with a sense of ‘constant burning and flares of electrocuting pain’ radiating up his neck, is caused when there is pressure or irritation to the occipital nerves in the back of the head. This can be because of injury, inflammation or muscles entrapping the nerves.
As a result of George’s rugby injury, many aspects of university are particularly challenging, especially on a course such as medicine, He revealed to Epigram that ‘attending practicals and placements can be a real struggle’. This is a problem that many students suffering from chronic pain must face. The condition and its impacts have also had a profound effect on George’s mental health.
George has tried many different treatment options to try and control his condition including a spectrum of pain medications, from strong opiates to pregabalin. He has also undergone more invasive therapies including several steroid, local anaesthetic and botox injections as well as radiofrequency ablation.
However, none of these have given much relief. Speaking with George, he described that: ‘The longest time pain free was five months, and cumulatively in the past 5 years I have spent about 10 months pain free.’
Resting and eating well enables him to manage the bad flare ups but ‘ultimately it is not a great quality of life.’ Therefore, George is currently fundraising £30,000 for a life-changing surgery.
Over 10 per cent of Bristol’s student population have a hidden disability, but how would you know?
New poster campaign is making invisible disabilities visible on campus
The surgery involves inserting a pacemaker-like generator into the chest, with a probe extending up to the occipital nerves in the neck. This probe will use tiny electrical shocks to block the pain signals being transmitted through the nerve, hopefully reducing, or even eliminating the pain to improve George’s quality of daily living.
A link to George's ongoing fundraising page can be found online here.
Featured Image: Unsplash/Aaron Blanco Tejedor
For those struggling with chronic pain, support is available from the University of Bristol Student's Health Service, Bristol pain clinic and your personal tutors.