By Edward Deacon, SciTech Digital Editor
A new study published by Bristol University suggests that vitamin D – and possibly vitamins K and A – could reduce the infectivity of SARS-CoV-2 by binding to the virus’ spike proteins.
A previous study undertaken by Bristol researchers showed that linoleic acid could bind to a specific part of the viral spike protein, changing it into a closed and less infective form. Closing the protein in this way inhibits its ability to interact with a certain human protein (ACE2) associated with infection.
The new paper, published in Angewandte Chemie, looked for new compounds that could replicate the same effect as potential preventative treatments against the virus.
Designing, developing and testing anti-viral drugs is a long process that can take years. Considering existing drugs and vitamins, and identifying those that could bind to the ‘druggable pocket’ inside the viral spike protein, would save time and make distribution easy given such compounds are already manufactured and widely available.
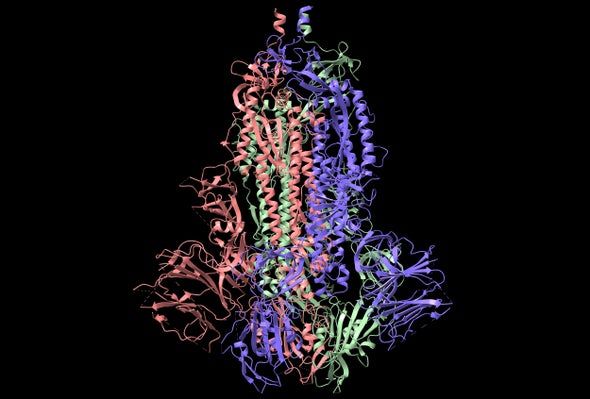
The researchers employed computational techniques to test different substances by simulating their response to the potential binding site. Several drugs were identified as being effective at potentially blocking viral replication through the manipulation of the spike protein.
Included in these were readily available pharmaceuticals and dietary components such as vitamins D, K and A.
Dr Deborah Shoemark, Senior Research Associate (Biomolecular Modelling) in the School of Biochemistry, who modelled the spike explained: ‘Our findings help explain how some vitamins may play a more direct role in combatting COVID than their conventional support of the human immune system.’
‘Obesity is a major risk factor for severe Covid’
However, she warns that the benefits may not be seen equally by everyone: ‘Obesity is a major risk factor for severe Covid. Vitamin D is fat soluble and tends to accumulate in fatty tissue. This can lower the amount of vitamin D available to obese individuals.’
Dr Shoemark also notes that a geographical inequity plays a role, saying: ‘Countries in which some of these vitamin deficiencies are more common have also suffered badly during the course of the pandemic.
‘Our research suggests that some essential vitamins and fatty acids including linoleic acid may contribute to impeding the spike/ACE2 interaction. Deficiency in any one of them may make it easier for the virus to infect.’
By binding with enough cholesterol molecules, the viral particles could infect human cells
In addition to the increased risk from obesity, high cholesterol levels have also been found to increase the risk of severe COVID-19.
Studies suggesting the viral spike protein binds to cholesterol lead the Bristol team to investigate whether it too could bind at the fatty acid site where linoleic acid and the other substances were found to.
Vaccines offer desperately needed hope, but they must be for everyone
Treatment for addiction: How are patients coping with the pandemic?
Dr Shoemark explained that the results suggested ‘by directly interacting with the spike, the virus could sequester [isolate] cholesterol to achieve the local concentrations required to facilitate cell entry’, that is, by binding with enough cholesterol molecules, the viral particles could infect human cells.
The research team consisted of experts from Bristol UNCOVER (University's COVID-19 Emergency Research) Group, including the Schools of Chemistry, Biochemistry, Cellular and Molecular Medicine, and Max Planck Bristol Centre for Minimal Biology, and BrisSynBio, using Bristol’s high performance computers and the UK supercomputer, ARCHER, as well as Oracle cloud computing.
Featured Image: PublicDomainPictures / Pixabay
Will you be topping up your supplies of vitamin D supplements?