By Julia Mullins, Second Year Politics and Philosophy
I went into anaphylactic shock in April of my first year of university. Somehow my closest friends at university had no idea I had an allergy, and the few who knew I carried an epi-pen didn’t know what I was allergic to. It was a pretty dire reality check for me.
Anaphylaxis is a life-threatening allergic reaction that progresses very quickly, potentially resulting in anaphylactic shock or in rare cases death. The UK has seen a drastic increase in anaphylaxis hospital admissions over the last twenty years, despite a fall in mortality rate. At 21 years old, I am in a very high-risk age group for managing my allergies, according to the charity Anaphylaxis UK. I believe the reasons why fatalities are most prevalent in the sixteen to twenty-four age group are exacerbated by social pressures, so I want to share my experience managing, or at least attempting to manage, a severe allergy whilst at university.
Being open about health conditions isn’t always easy. Especially not while navigating a new environment and desperately trying to make a good impression on your flatmates. As a child, your condition is most likely monitored by parents and your school. Moving to university forces you to be responsible for managing your allergy alone and educating the people you live with. Restricting what is allowed in the kitchen, asking flatmates to check ingredient labels, and vigilance about possible cross-contamination are essential to keeping me safe. Despite this, I was reluctant to impose on my flatmates and could never seem to find the right time to bring it up.

Months later, I was having dinner on a summers evening with friends. I knew immediately that something was wrong. But without knowing how severe it would be I didn’t want to alarm anyone. The constant fear of anaphylaxis makes me vigilant about noticing the onset of symptoms, but this paranoia can also feel like an overreaction. Once I eventually spoke, my friends sprinted into the kitchen, scrambling to read ingredients. Having spent years at school together they knew exactly what to look for. The conviction and speed with which they acted was remarkable. They rang 111, 999, knocked on neighbours’ doors and contacted my parents – thankfully ignoring my protesting. Unfortunately, the Epi-pens I should have been carrying had been forgotten in the bottom of a bag somewhere at home. By the time I sincerely thought I could die (also a symptom of anaphylaxis), paramedics were at the door.
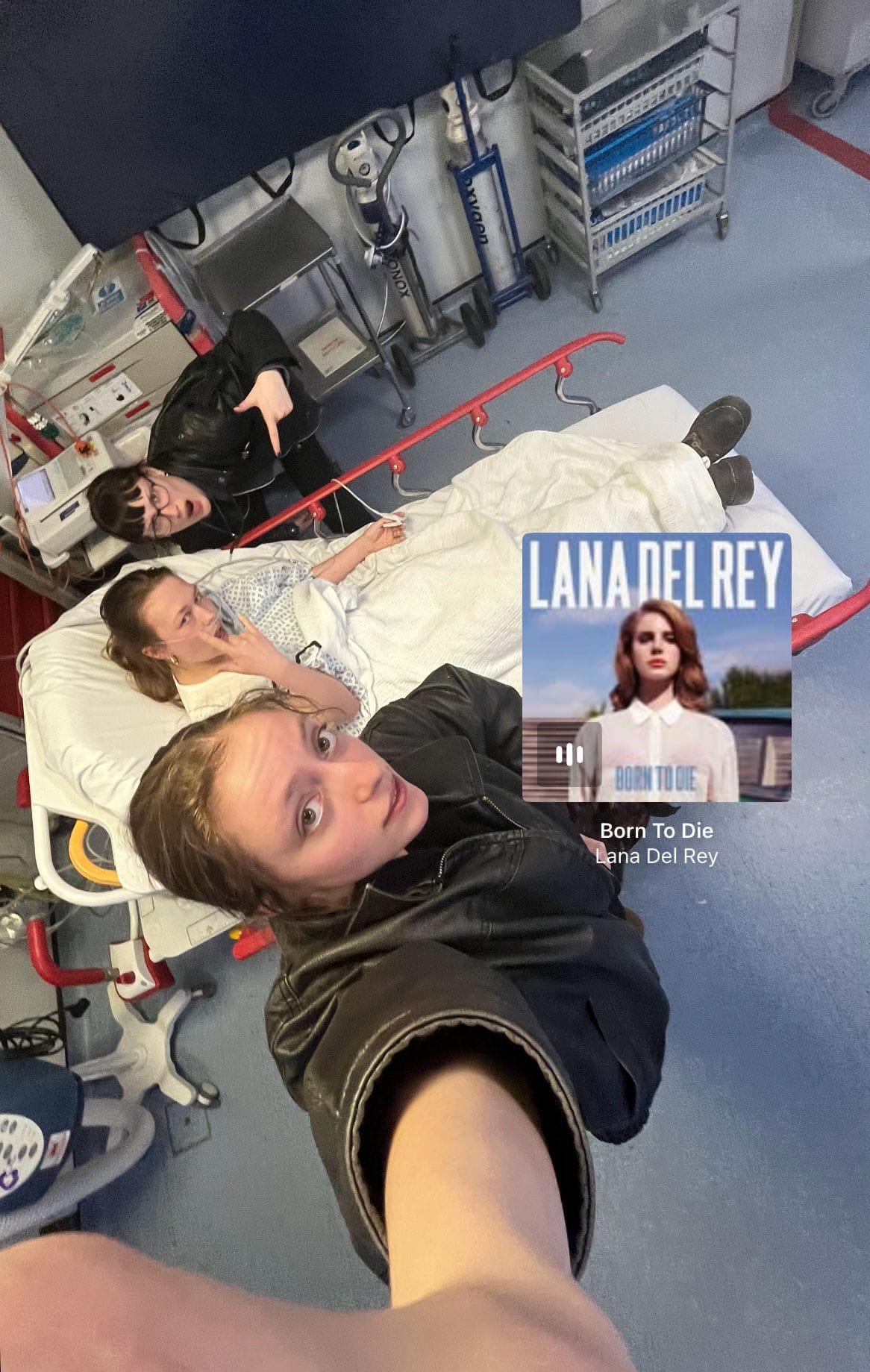
I don’t remember much of it, I know there was a lot of throwing up involved. When I couldn’t see or hold up my head any longer I curled myself up on the floor, thinking about dying and breathing. There was a moment in the ambulance where my whole body was shaking from multiple administrations of adrenaline that it looked like my legs, stretched out on the bed, were trying to walk away without me. I was hooked up to all the things: needles, wires and masks, along with a constant murmuring of paramedics speaking in their acronyms. My friends stayed by my side for as long as they could and returned for visiting hours the next day. Much of the night spent alone was filled with phone calls from family trying to cheer me up and posting Lana del Ray’s ‘born to die’ on my Instagram story.

After having my hospital stay extended multiple times, someone pressed a prescription into my hands and I was suddenly discharged. Having arrived by ambulance, I got halfway down the corridor before realising I had no idea where I was. Exhausted and in tears I left the hospital alone.
It’s no secret the impact anaphylaxis has on the quality of life and mental health of patients. Patients with anaphylaxis are more likely to have PTSD and associated psychological distresses, like anxiety and depression. Conditions involving strict dietary adherence have also been associated with an increased risk of a broad range of disordered eating behaviours. Over half of people living with allergies in the UK regularly avoid social situations due to their allergies and also feel they should minimise the extent of their allergies to the people around them, fearing judgement. This psychological impact is pressing because stress can intensify the symptoms of allergies, and reactions are likely to be more severe after your first experience of anaphylactic shock.
Six months after my stay in hospital, I was alone in a hospital waiting room for an unrelated routine appointment and completely broke down. It was the first time I had been forced to confront the experience I had gone through, and my own reaction shocked me.
It was made resoundingly clear to me by everyone that I should’ve had my epi pens with me. Two. At all times. Though I had been prescribed epi pens, I had never used one before, and for a few years had been particularly lucky - so I got complacent. I truly didn’t think anything would happen to me. Those between the ages of sixteen and twenty-four are likely to resist carrying adrenaline auto-injectors (commonly known by the brand name as Epi-Pens) and take greater risks experimenting with foods they are allergic to. Add to that the likelihood that any self-respecting uni student will be doing their fair share of drinking, so say goodbye to risk perception.
But this isn’t surprising, teenagers and young adults commonly present non-compliance to self-care behaviours, like carrying vital medication. An epi-pen isn’t the kind of drug you want to be sneaking into a night club.
I felt deeply that I was to blame for the whole ordeal, which in part I was. As an adult it is undoubtedly your responsibility to manage your condition. To tell your close friends and the people you live with, have awkward conversations at restaurants on first dates, check the ingredients, to set up emergency contacts, and to always carry two epi-pens with you. But also, know that it’s no mean feat, there are genuine psychological impacts of living with anaphylaxis, and that help is available.
Shame and reluctance when managing a severe allergy, is a real risk. For flatmates and friends, supporting someone with a severe allergy goes beyond dramatized emergency scenarios, make sure to leave room for honest dialogue too.
And for those who are wondering, the culprit was buckwheat.
For any further information, it’s recommended you speak to your GP but I have found the following charities to be helpful:
Anaphylaxis UK: ‘Going to University Guide’
Allergy UK: webpage titled, ‘Universities and Higher Education’
Advice and Support are also available from:
Anaphylaxis UK helpline 01252 542029
Allergy UK helpline 01322 619898