By Isabel Rowbotham, MSc Translational Cardiovascular Medicine
Private payers undergoing cardiac surgery may have a lower risk of mortality and post-operative complications compared to National Health Service (NHS) patients. The investigation on the impact of health inequalities on clinical outcomes was led by NHS cardiac surgeon and associate Professor at the University of Bristol, Dr Umberto Benedetto, along with colleagues and researchers from the Bristol Heart Institute (BHI).
The study analysed 280,209 patients who underwent cardiac surgery in England from 2009 to 2018. It is the first study in the UK which focused on ‘payer status’ as a risk factor in cardiac surgery outcomes.
‘Our findings support the hypothesis that a complex interaction between socioeconomic and health system-related factors exists for patients undergoing cardiac surgery’, explained Dr Arnaldo Dimagli, joint lead author and Honorary Research fellow at the University of Bristol.
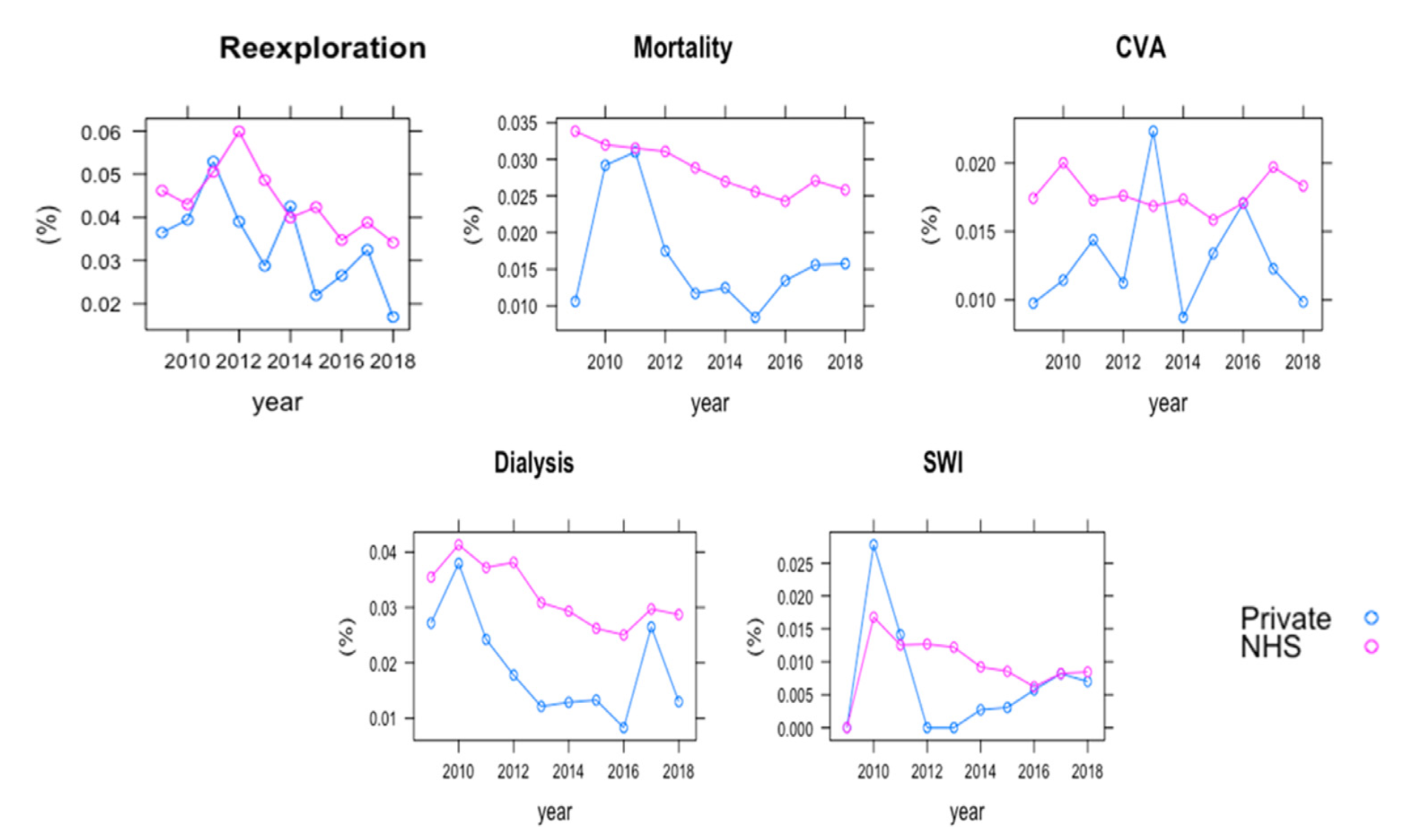
Private payers had a 21 percent lower risk of hospital mortality compared to NHS patients. Private paying patients were associated with the least deprived neighbourhoods, marking a clear disadvantage for NHS patients, although more so in elective procedures. Surprisingly, the study also identified that individual surgeons and hospitals could be attributed to higher mortality rates. It was observed that 15 percent of surgeons were associated with a 45 percent higher mortality, compared to patients who were not under their care.
When the researchers further looked into the relationship between payer status of the patients and the occurrence of postoperative complications from cardiac surgery, they found that private payers also benefited from lower risk of complications, including a lower incidence of later heart attacks.
15 percent of surgeons were associated with a 45 percent higher mortality, compared to patients who were not under their care.
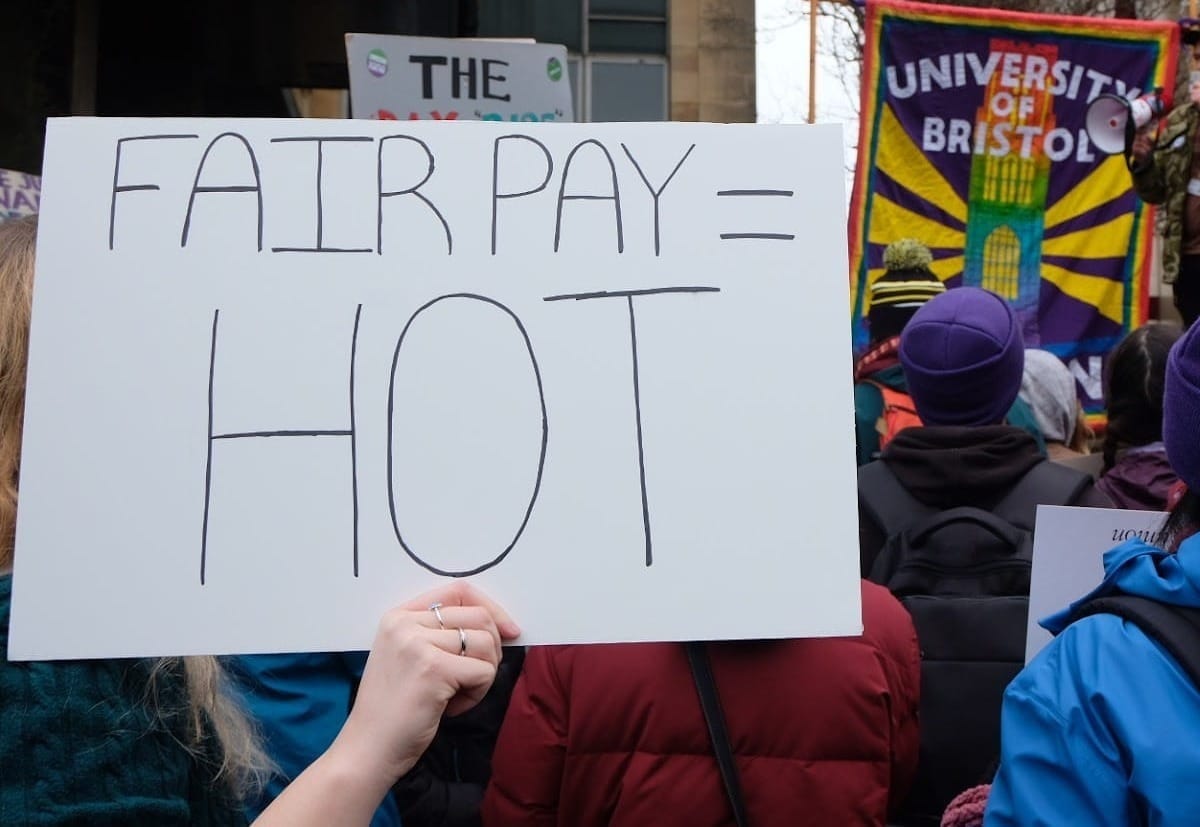
An equal distribution of socio-economic and environmental factors in the healthcare setting matters. In a country with a taxpayer universal healthcare system these inequalities can still be felt and are quantifiable. In this study, the socio-economic deprivation was measured by the UK Index of Multiple Deprivation (IMD) and is based on a person’s neighbourhood deprivation by indices evaluating income, employment, education, among other factors.
Reducing these health inequalities are key to lowering the risks which plague patients from more deprived and poorer neighbourhoods. Some of the reasons these increased post-surgery risks may be prevalent to NHS status patients are due to the increased burden of co-existing conditions. Another important factor to consider is that non-elective procedures commonly take place in NHS hospitals. This means that even if a patient may attend a routine surgery in a private hospital, in the event of an emergency the patient is likely to be transported to an NHS hospital instead.
Private payers also benefited from lower risk of complications, including a lower incidence of later heart attacks
On the other hand, private healthcare users have many reasons for their higher benefits on surgical outcomes. Private users tend to have earlier accessibility, shorter waiting times, are free to choose their surgery dates and have more comfortable facilities during their stay.
Unintended or pre-existing bias is another problem which clinicians may face in service delivery. Researchers suspect that individuals from deprived neighbourhoods may be at risk of communications problems, including difficulties understanding basic information regarding health decisions. Some known instances of these barriers are understanding the risk of unhealthy lifestyles and the under usage of preventative services, such as vaccinations and screening. The NHS have made an effort to improve the issue of health literacy, in an effort to treat all patients equally. Researchers suggest further improvements are needed in the service delivery of cardiac surgery and across other healthcare services.
Novel study highlights varied colorectal cancer risk between sexes
Vaccines offer desperately needed hope, but they must be for everyone
This study highlights that payer status matters, in terms of survival and clinical outcomes of cardiac surgery patients. The study’s strengths lie in the usage of large data, including 280,209 patients spanning over this past decade. Although, it is not clear if payer status also has an effect on the cause of death and not just its incidence, as this aspect was not part of the analysis.
Overall, there is a significant benefit for opting for private services in terms of cardiac surgery outcomes, though understandably not everyone can afford it. Therefore, it is evident that further work is needed in order to reduce the socio-economic and health inequalities amongst healthcare patients.
Featured Image: Epigram / Isabel Rowbotham
How could we raise the standard of the NHS healthcare system to that of private UK hospitals?