By Gwen Morgan, Third year, Biochemistry
You’ve packed all your bags for uni: stationery, décor, towels… condoms? Let’s be honest, Freshers’ week has a certain reputation. Whether or not you choose to get involved, feeling sexually safe and confident is a skill worth mastering. Think of this as your first unofficial assignment: figuring out what safe sex means to you.
“Here's one I tried earlier”
Imagine you’ve had a fun night and your date suddenly leaps up and starts hopping around. Don’t let this get to your head, they may not be celebrating - ancient Greeks believed hopping backwards seven times after sex could prevent pregnancy. Meanwhile, ancient Egyptians were busy making contraceptive paste from honey, sodium carbonate… and crocodile dung (romantic, right?). History is full of questionable attempts: lemons as diaphragms, Coca-Cola as spermicide, even drinking liquid lead or mercury. Much to our relief (and their despair), such lengths are neither effective nor necessary… and neither are weasel testicle garters (unless you’re into that type of thing) - though they’d make a great conversation starter at a medieval costume party. Luckily, modern contraception is not only far less obscure - it’s also far more effective. No longer must animal bladders be all that stands between you and a flat baby.
The pill, the patch, and the patriarchy
The trajectory of contraception development was undeniably influenced by the patriarchy and outdated traditional values, leaving a burden of responsibility on women.
In 1961, British women could get the first hormonal birth control pill, though initially only if they were married. This was overturned in 1967 and emergency contraception eventually became available in 1984. Along the way, creative attempts continued in the form of sponges, pessaries and spermicides with varying degrees of success.
The evolution of male contraception is much shorter and simpler. Linen cloth and animal organ condoms were transformed by rubber in the 1840s and perfected with latex in the 1930s. They remain the primary form of male contraceptive, preventing both pregnancy and infections. There are now many forms of female hormonal contraception: injections, patches, implants and IUDs (both copper and hormonal).
Coming soon
If history shows anything, it’s that human creativity knows no limits when it comes to sex. And innovation isn’t slowing down. On the near horizon we can expect new delivery systems like contraceptive gels, vaginal rings, and skin patches - no more 'oops, I forgot my pill.' Beyond this development is in progress for selective hormonal modulators with reduced side effects, 'once a month' pills that inhibit implantation (again less need to remember) and contraceptives that double as STI protection through built-in antiviral agents.
The development of contraception has been heavily influenced by the patriarchy and gender roles, often leaving women to take responsibility for everyone’s reproductive health.
Innovators are now looking to make men’s contraception a bit higher tech than what is essentially a plastic bag, beginning a long overdue shift. There are hopes for a non-hormonal pill that blocks sperm production, hormonal gels to inhibit sperm production and sperm duct blocking gels like ADAM or Plan A administered in a reversible but long-term procedure which remains less invasive than many female equivalents. The future looks promising for contraception that is smarter, safer and way less hassle.
Safety first!
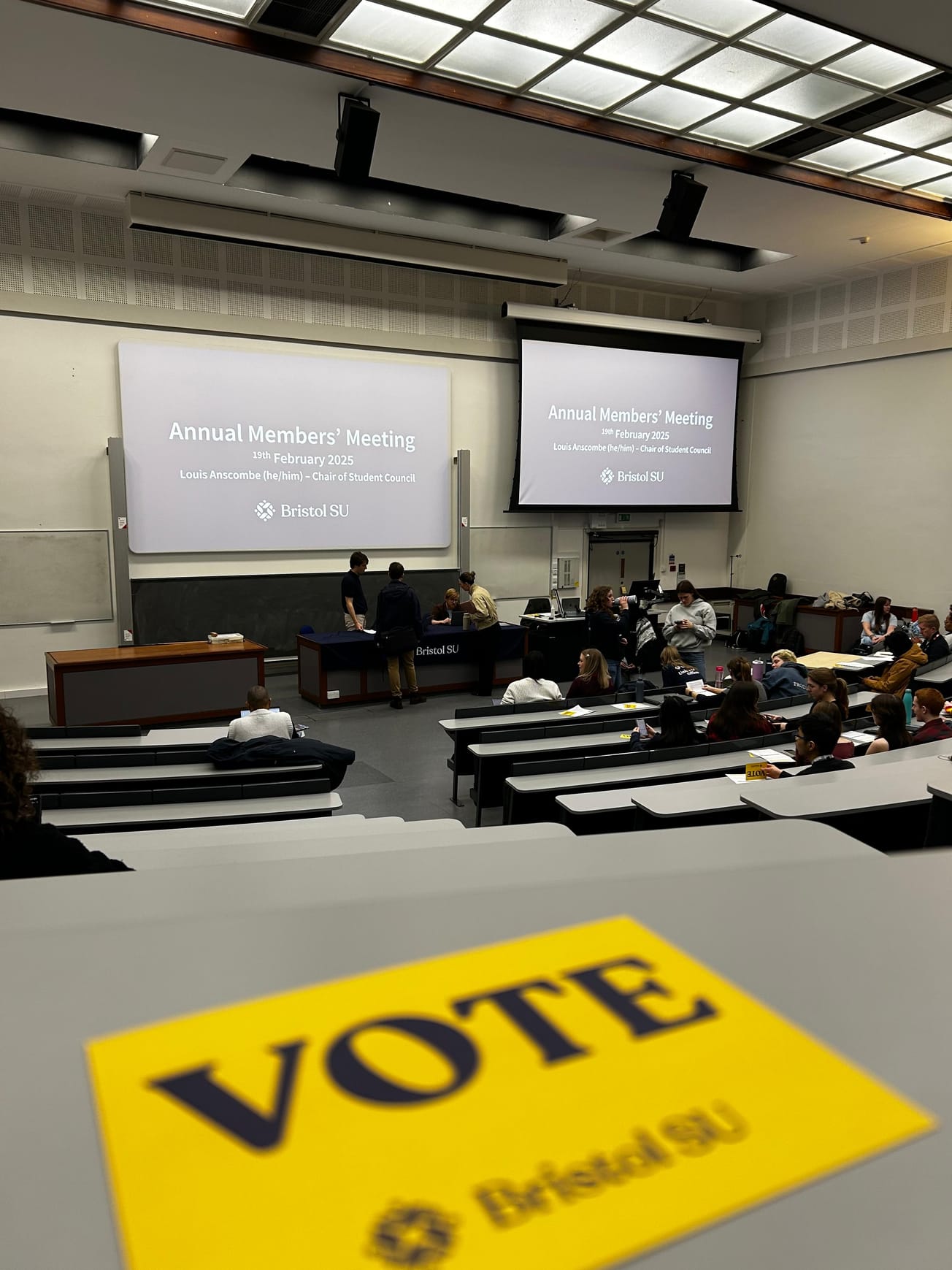
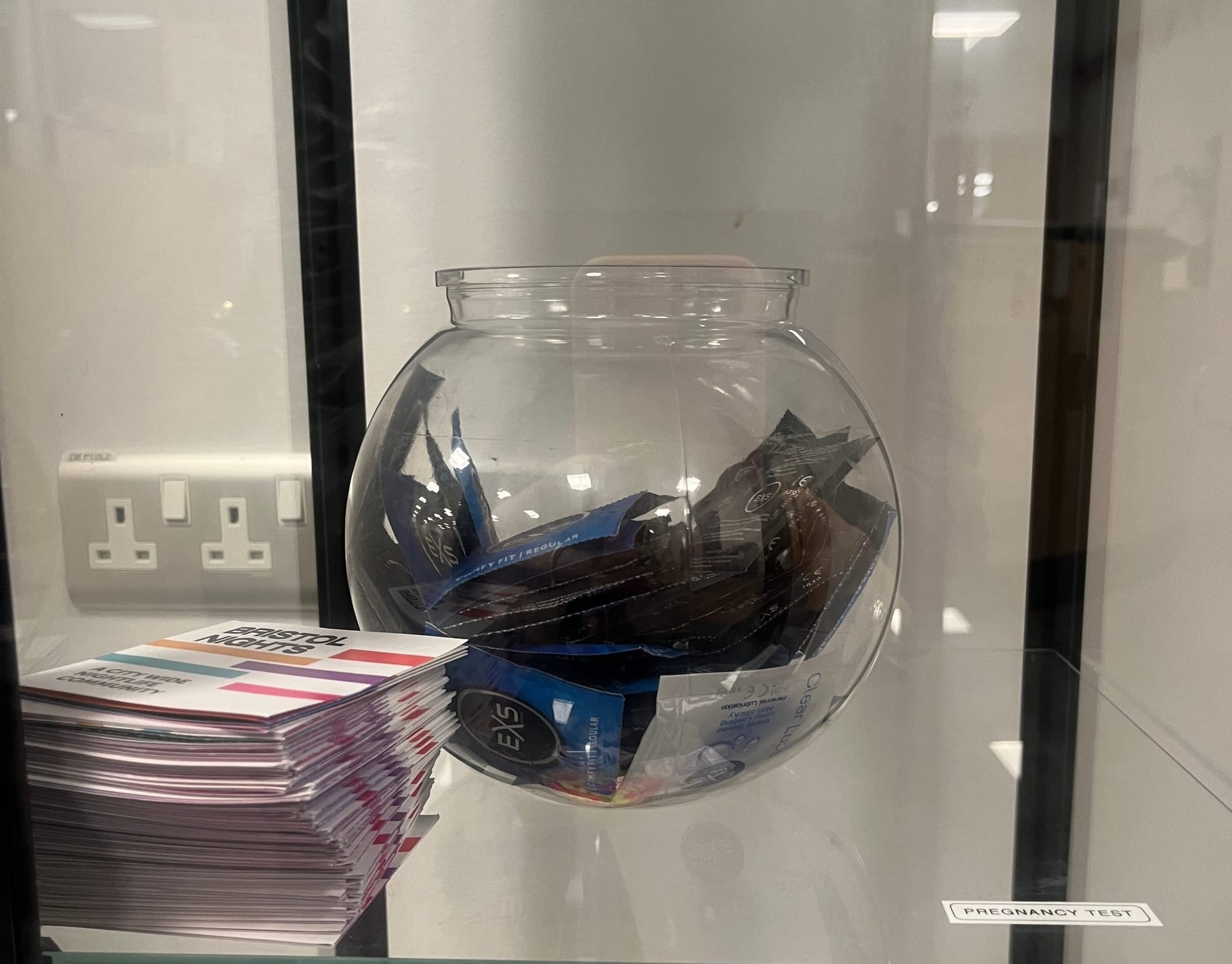
Whether it’s for peace of mind, preventing pregnancy, or avoiding STIs, safe sex is about empowerment, not fear. University is a time of exploration, and whatever choices you make you deserve to make them safely. Contraception is available for free via Brook services, contraception clinics and sexual health clinics. Condoms are available for free online order from Yuno, in the waiting room of the Student Health Service and as part of the university’s sexual health provisions from the Community Cabinet, located on the 5th floor of Senate House, alongside pregnancy tests. If you have had unprotected sex or your primary method of contraception has failed, emergency contraceptives (pill or copper coil) are available through your GP or sexual health clinics. STI test kits are widely available from free vending machines around Bristol, for women in the Student Health Service waiting room (pink and white striped bags) or by post so that you can test at home. If you’re more comfortable with an appointment ,the Unity Sexual health clinic is a welcoming and confidential environment.
So, date, have some fun, make some questionable decisions… but let's keep the surprises to a minimum and, hey, if you don’t, its okay, at least modern tech has got your back. No fizzy beverages or animal remains will be going anywhere but your mouth.
Featured Image: Epigram / Kimberley Goh
Do you think students are aware of the available sexual health services?