By Julia Riopelle, Second year, Zoology
March is Brain Tumour Awareness Month. Brain tumours are very aggressive and their initial diagnosis is difficult, but new research may be able to change that.
According to the Brain Tumour Charity, 5,000 of the 11,700 individuals diagnosed with glioblastomas die annually. Current statistics show that only 11% of those diagnosed with primary brain tumours in the United Kingdom survive five years post-diagnosis, and those which do have an estimated reduction in life expectancy of approximately 20 years. Brain cancer is one of the most aggressive forms of cancer with the highest mortality rates.
Glioblastomas are malignant tumours occurring in the brain and spinal chord. Survival times are approximately three months if they are left untreated. Initial diagnosis of suspected brain tumours is difficult, as many warning signs - such as headaches, nausea or vision problems - can be attributed to many other illnesses.
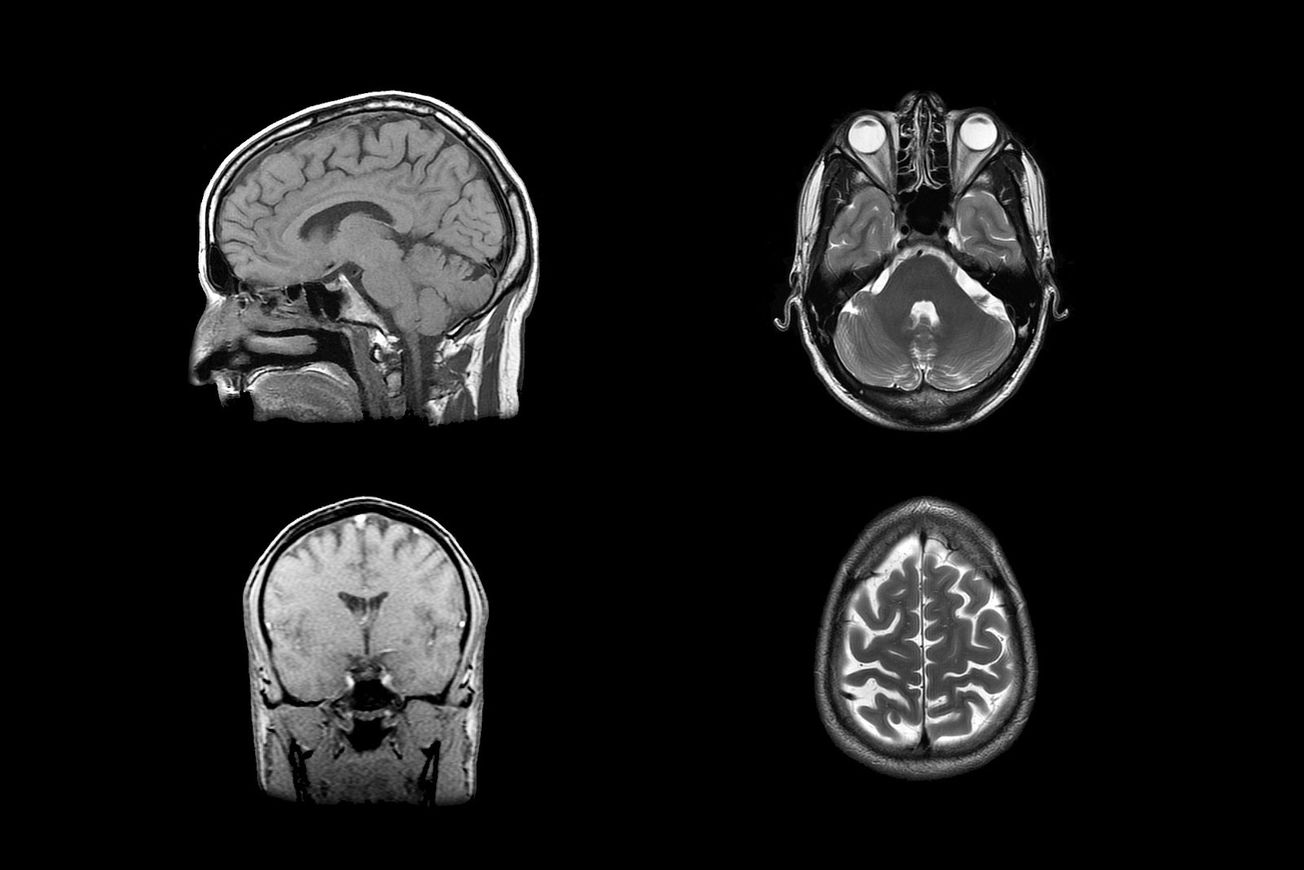
Currently, practitioners diagnose brain tumours through initial neurological exams, such as testing vision, hearing, coordination and reflexes. Imaging tests are also commonly used, such as magnetic resonance imaging (MRI) and computerised tomography (CT) scans. Biopsies can be taken during brain operations, however such invasive procedures are accompanied by higher risks.
Today is the start of Brain Tumour Awareness Month. Throughout #BTAM we’re bringing you stories from our community. From those living with side effects, those battling treatments & those who have sadly been lost.
— The Lewis Moody Fdn (@LewisMoodyFdn) March 1, 2020
Let’s be brain tumour aware & together we can #TackleBrainTumours pic.twitter.com/kD6jSr8WFC
Despite the causes of brain tumours being largely unknown, it has been observed that a mutation in the TP53 gene coding for the tumour suppressor P53 is often prevalent in glioblastoma patients. Cellular division is a necessary and natural part of the cell cycle, required to periodically replace somatic cells in the body with new ones. Its phases are initiated and halted by molecule complexes known as cyclins and cyclin-dependent kinases (CDKs).
P53 is a regulatory subunit of CDKs, known as the tumour repressor, as it inhibits the transcription of certain cyclins responsible for the initiation of mitosis. Mutations in the TP53 gene, causing a lack of P53, are one of the most common causes of cancer, leading to uncontrolled mitosis and the development of tumours.
A multidisciplinary collaboration between researchers at the University of Bristol, Brain Tumour Research and the Bristol start-up FlouretiQ Limited are developing a blood test aiming to detect brain tumours. This project is led by Dr Kathreena Kurian, an Associate Professor in Brain Tumour Research and Dr Sabine Hauert, a Senior Lecturer in Robotics. It also requires the expertise of Co-Investigators, Professors Carmen Galan and Richard Martin from the University of Bristol, and ongoing assistance from Dr Neciah Dorh at FlouretiQ Limited and Dr. Helen Bulbeck from Brainstrust.
Dr Kathreena Kurian,
— Bristol University 🎓 (@BristolUni) March 8, 2020
Head of the Brain Tumour Research Centre, shares her thoughts on #IWD2020 https://t.co/3Bz4pu5MVu
The blood test uses a combination of fluorescent carbon dots (FCDs) and nanophotonics in order to detect tumour biomarkers. Biomarkers are chemical substances, such as proteins, DNA or micro-RNA, which are secreted by cancerous cells. As glioblastomas invade the surrounding primary tissue and cause lesions in the nearby blood vessels, biomarkers can be detected in the bloodstream for early tumour diagnosis.
One such biomarker is glial fibrillary acidic protein (GFAP), a protein which creates intermediate filaments which form support networks to astroglial cells, which assist the absorption of neurotransmitters and maintain the barrier between blood and brain. However, GFAP levels tend to be too low for detection via antibody assay techniques, such as ELISA. Thus the team hopes to also find other more suitable biomarker options.
| The urgent need to STEMpower women
In collaborating with FlouretiQ Limited, the team is developing affordable fluorescent carbon dots (FCDs) in order to test patient’s blood. These are an upcoming class of nanoparticles with ‘high chemical stability, biocompatibility, low toxicity, resistance to photobleaching and easily modified’, according to a paper in 2014. Due to their high surface area to volume ratio, they are able to bind to many types of molecules, some of which can recognise specific cancer molecules and will specifically target them. The binding of these compatible ligands can emit fluorescence, which can be detected via assays under UV light.
| Yes we can-cer: shrinking tumours by boosting the immune system
However, a limitation of solely relying on biomarkers is that they often occur at low levels in the blood. Therefore, the FCDs will be detected with enhanced nanophotonic technology. Nanophotonics studies the behaviour of the emitted light on a nanometer scale and thus allows highly sensitive detection. This non-invasive diagnosis method would be game-changing in the time-sensitive race of treating brain cancer, possibly saving countless lives in the near future.
The project is generously sponsored with the investment of £500,000 from Cancer Research UK, with the hopes that this blood test will speed up diagnosis and treatment action. If successful, it would drastically increase chances of survival before the tumour metastasizes, as well as improve the monitoring ofthe possibility of post-remission relapse.
Featured image: Flickr / David Foltz
Want to write about your research? Get in touch!