By Julia Riopelle, SciTech Editor
A meta-analysis of 52 published studies has found that, globally, Intensive Care Units (ICU) mortality rates due to COVID-19 have significantly decreased since the start of the pandemic, though improvements are now beginning to plateau.
The newest UK governmental reports from the 24th February state that there have been 9,938 new daily positive cases and 442 new deaths of patients within 28 days of testing positive for the virus. Despite these harrowing numbers, there is some hope to be seen – the national lockdown is working.

A meta-analysis, led by Professor Tim Cook, consultant of Intensive Care Medicine at the Royal United Hospitals Bath NHS Foundation Trust and Honorary Professor in Bristol Medical School: Translational Health Sciences (THS), looked at the outcomes of 43,128 ICU patients across North America, Europe, the Middle East, China, Australia and South Asia.
A previous meta-analysis, conducted by Cook and his colleagues (linked below), showed that ICU mortality rates fell from 60 percent at the end of March 2020 to 42 per cent at the end of May. The new meta-analysis has found that as of October 2020, ICU mortality has further decreased to 36 per cent.
Despite the improvement, the rate of decrease has clearly slowed down. Between March and May, a period of two months, ICU mortality rate dropped by 18 per cent. However, from June to October, a period of five months, mortality rates only decreased a further six per cent. The plateauing decrease is also concerning, as the data of this study is only up until October and does not consider the impacts of increased cases over the winter season, as well as the pressures the new UK, South African and Brazilian strains have added.
In January of 2021 alone, the NHS had admitted 101,956 new COVID-19 patients, accounting for 29 per cent of total admissions since the start of the pandemic. As a result, the number of patients which had to be admitted into hospital between December 2020 and January 2021 also increased by 79 per cent.
In January of 2021 alone, the NHS had admitted 101,956 new COVID-19 patients
The study found that improved treatments were not a confirmed reason for the overall improved ICU management between March and October. However, some did find evidence supporting that steroids helped improve the survival of patients who required respiratory support. Other management changes in ICU approaches to fluid therapies, oxygen support and response to blood clotting have also become systematically improved.
As the pandemic progresses, hospitals and virologists have more exposure to the virus’ symptoms, and therefore ICUs may have become more prepared for various outcomes. Whilst most ICU mortality rates remain between 30 to 40 per cent globally, some countries are experiencing better outcomes than others. For instance, hospitals in Melbourne are at an average ICU mortality rate of 11 per cent, whilst the Middle East is experiencing a higher mortality rate of up to 62 per cent.
The stark contrast across these mortality rates may be due to differences in what constitutes an ICU and which patients qualify for it. This may well be related to the socio-economic status of the area the hospital is located in and the resources available to them.
If resources in the Middle East are more limited in comparison to wealthier, geographical areas, they are likely to only admit the ‘worst of the worst’ into the ICU. This may explain why their death rate is at 62 per cent– as those patients admitted are in critical condition. Wealthier areas, such as Australia, may have the resources to admit more patients into their ICUs – not only those at the highest risk of succumbing to the virus – and therefore may appear to have lower mortality rates.
The contrast across these mortality rates may be related to the socio-economic status of the country
It is nevertheless clear, that those admitted to ICUs are disproportionally sicker than those in other hospital units. In other units, ‘advanced non-invasive respiratory support’ is administered to non-critical COVID-19 patients, meaning that only those in the ICUs require invasive ventilation. To combat the pressures on ICUs, which experienced up to 90 per cent mortality rates in the early stages of the pandemic, the units have to be extremely selective on who they admit.
Interestingly, the study did not find higher ICU mortality rates to be correlated with the number of people admitted. One of the studies analysed from April 2020, which included 371 patients in New York, admitted 100 per cent of their patients into the ICU. Of these patients, 78 per cent died. However, three studies published in May of 2020, showed that hospitals in Atlanta, Indianapolis and Vancouver admitted 96, 97 and 90 per cent of patients into their ICUs, respectively. Despite around the same percentage of patients admitted into the ICUs as in New York, those hospitals reported much lower mortality rates of 30, 26 and 17 per cent, respectively.
The units have to be extremely selective on who they admit.
There is light at the end of the tunnel. Improvement is still improvement, no matter how small. Even in the UK, a nation which has been battling the pandemic with immense difficulty since its start, has recently seen positive trends. Since the peak number of new daily COVID-19 infections at the start of January, daily cases have been dropping substantially every week.
On a 7-day average (last recorded on 18 February 2021), Bristol is still testing 122.6 people positive per 100,000 for COVID-19. Neighbouring areas of Bath and Mendip are testing much less, reaching a 7-day average of 50.7 people per 100,000. Currently, we are just below the level of cases as we have had at the end of November. It was also reported that the R-Value is now between 0.6 to 0.9, a range we have not seen since July of 2020.
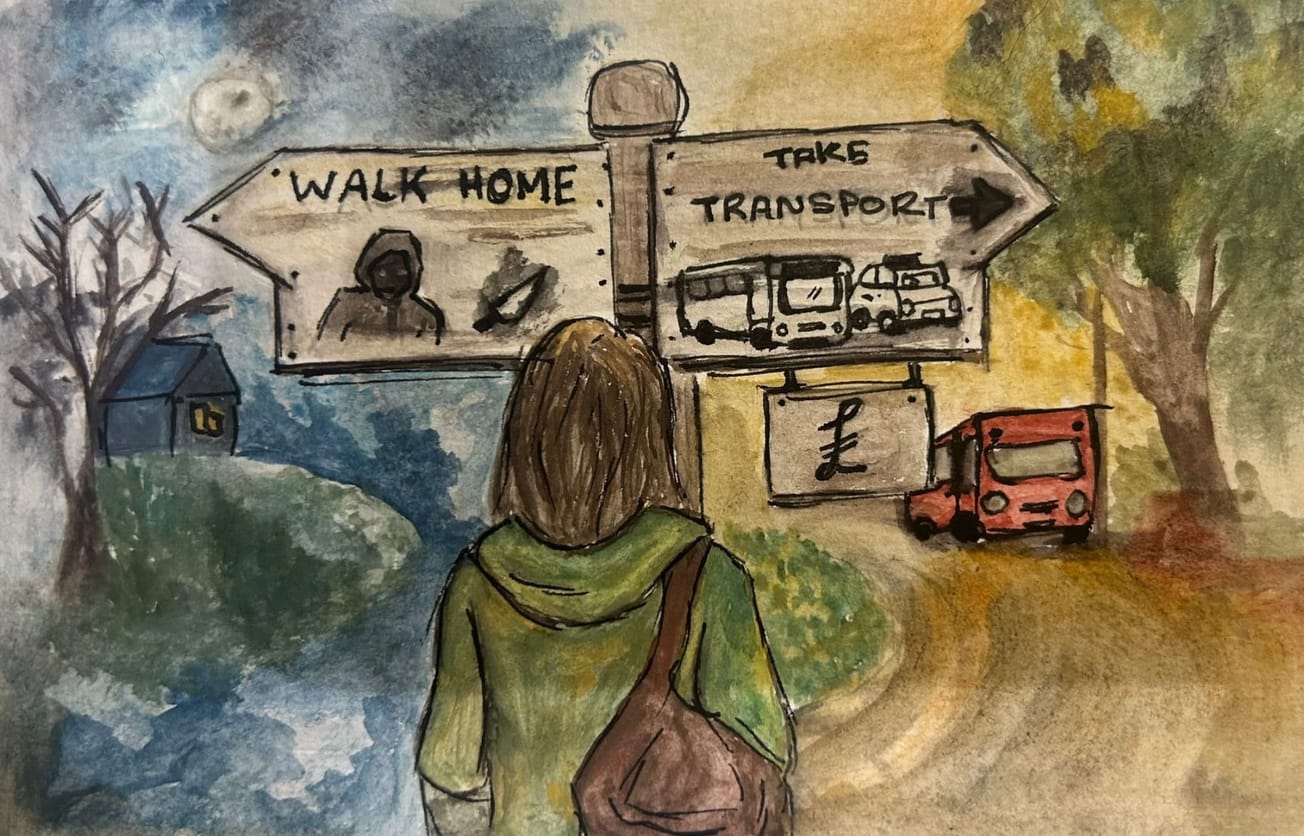
Over 14 million people have now received their first vaccination and the #transport industry continues to play a vital role in helping people get their vaccines.
— Dept for Transport #StayHomeSaveLives (@transportgovuk) February 13, 2021
Find out how transport is helping in the fight against #COVID19 here 👉 https://t.co/u04xM06h3e
#COVIDVaccine pic.twitter.com/R2PupPXisD
An R-value is a measurement of the infection rate of a virus, specifically the number of people one individual is infecting. Any value below 1.0 indicates that the infection rate is decreasing. This is due to a combination of lockdown and protection offered by the vaccine.
Currently 18,242,872 have received the first dose of one of the three approved COVID-19 vaccines in the UK (Pfizer, Oxford-AstraZeneca and Moderna), whilst 669,205 have received their second dose. This is around 27 per cent of the UK population.
University of Bristol involved in international COVID-19 study on ICU mortality
Online guide launched to inform and fight misinformation to help ‘share facts, not fiction’ about COVID-19 vaccines
We must remember that this pandemic is not over – though we are all growing restless of it. This lockdown is successfully achieving what it has set out to do, however we are still not at the numbers we need to be. So, we must continue to stay at home and socially distance where we can. It is our job to collaborate in keeping everyone safe and alleviating the pressure currently on our Intensive Care Units.
Warning, graphic content: The New York times published a video about an ICUs as seen by nurses.
Featured Image: Unspash / Li Lin
Do you think the UK is on the right track or do they need to do more?