by Lilli Waples, MScR Psychology
Early insights from the University of Bath and Bristol’s What C-OST? study have provided some insight into how people receiving Opioid Substitution Therapy (OST) for opiate addiction are coping with the impact of the pandemic on their treatment.
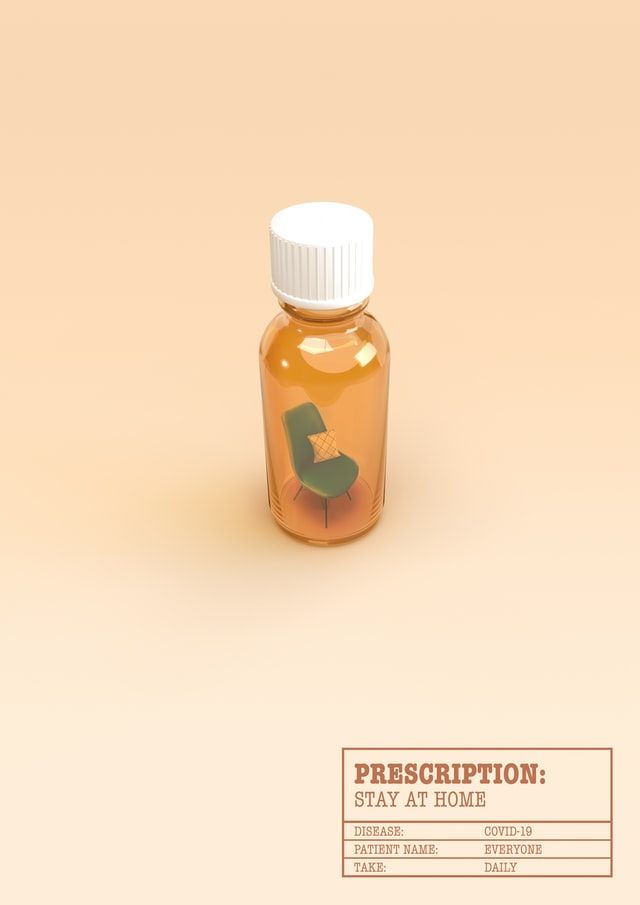
Under normal circumstances, a person in receipt of OST would need to make daily trips to the pharmacy in order to receive their medication under the careful supervision of a pharmacist, as a means of reducing overdose and drug-related deaths. However, during the pandemic patients have been supplied with enough medication to last one or two weeks at a time, in order to minimise contact between patients and pharmacists and to reduce the necessity for patients to travel.
What C-OST? is a qualitative interview study led by Dr Jenny Scott, from the University of Bath’s Department of Pharmacy and Pharmacology, seeking to understand the impact of these changes for patients receiving OST.
As of November 2020, six people have been interviewed for the study so far. The majority of interviewees have reported coping fairly well with the change in prescribing practices. All of the participants have reported being able to manage their own medication and not take more than their prescribed dose. Furthermore, a number of participants have welcomed reduced trips to the pharmacy as it affords them more freedom to go to work or care for their families, as well as saving money on public transport.
These findings are promising, however Dr Scott points out that for some people, taking home large quantities of their medication may not be appropriate as it may facilitate overdose or relapse into street drugs.
‘I think we need to have an effective way to identify the different levels of care and support people need’ Scott argues. ‘A one size fits all model does not seem to work, so [we need] a way of identifying who needs tight controls over medicines and face to face support versus who can have a more 'light touch' support and get on with their lives. More work is needed to understand this.’
In addition to the changes in prescribing practices, patients are having to get used to a loss of face-to-face contact with their addiction recovery services. While many people are struggling with loneliness during the pandemic, this is particularly challenging for people experiencing addiction. Feeling isolated can cause their mental health to suffer, making recovery more difficult.
‘Some have found it easier to avoid others who may lead them to use drugs, so have stayed home, and reduced their drug use or detoxed, although they have been isolated and lonely. Others have struggled and found their drug use hard to manage in isolation and their mental health has suffered.’
Going forward, Dr Scott and colleagues are aiming to recruit an additional 24 people for this study. She is also collaborating on the LUCID-B study led by the University of Bristol, examining the effects of the pandemic on people who inject drugs in Bristol. It is hoped that both of these projects can help to inform future drug treatment policy by exploring how patients respond to such significant changes in their lives and treatments.
Featured image: Christina Victoria Craft/ Unsplash







